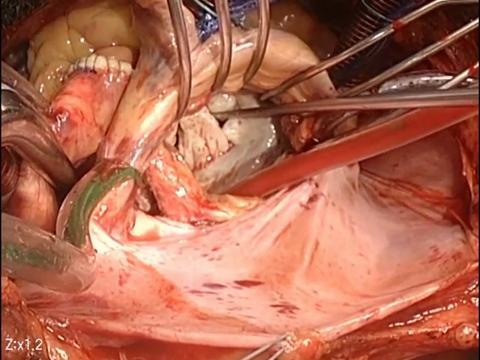
Hypertrophic obstructive cardiomyopathy (HOCM), historically referred to as idiopathic hypertrophic subaortic stenosis, is a relatively common disorder. HOCM is a significant cause of sudden cardiac death in young people, including well-trained athletes, and affects men and women equally across all races.
In most patients, it results from asymmetric septal hypertrophy causing outflow obstruction of the left ventricle. It is difficult to diagnose and presents a challenge to medical health professionals in evaluating at-risk athletes. This activity reviews the evaluation and management of hypertrophic obstructive cardiomyopathy and highlights the role of interprofessional team members in collaborating to provide well-coordinated care and enhance outcomes for affected patients.
- Fortis Hospital Shalimar Bagh, Delhi
- rajuvyas63@hotmail.com